Companies news
From health-for-all to health-for-wealth. Asia-Pacific's healthcare financing needs a rethink

The Asia-Pacific (APAC) region is home to the majority of the world’s population and is expected to contribute to roughly 60% of global growth by 2030.
The idea of “health is wealth” means that a healthy population will determine whether many APAC countries can make or break the middle-income trap. With that, ensuring individuals and communities have access to the healthcare they need without suffering from financial hardship, has been at the forefront for most of the region’s governments.
However, the region is faced with unprecedented pressures that challenge delivery and financing models of existing healthcare systems. These challenges include: ageing populations; the rise of communicable disease coupled with the continued menace of non-communicable diseases; and the barriers to achieving Universal Health Coverage (UHC).
The traditional approach to rely mostly on either income tax or social health insurance contribution for health system financing has also proven to be inadequate and unsustainable. Few countries in APAC achieve the 15% Tax-to-GDP ratio, for example, the critical threshold set by the IMF to support sustained and inclusive growth.
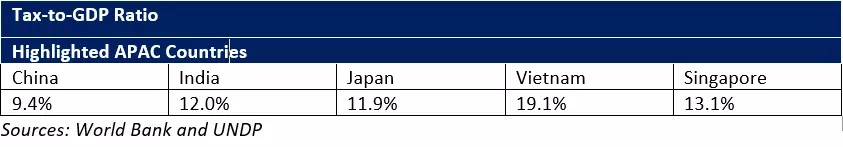
Image: World Bank/UNDP
Furthermore, the greying population is expected to shrink the available taxable workforce, while a large informal economy further limits countries’ ability to raise the requisite financing for their health systems.
As a result, many APAC governments have difficulty financing their healthcare systems, resulting in high out of pocket healthcare expenditure among citizens and serving as one of the leading causes of poverty.
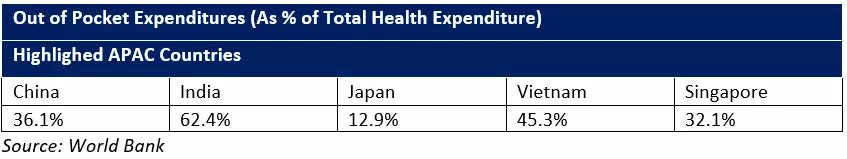
Image: World Bank
The ongoing COVID-19 pandemic has further unveiled the fragility of regional healthcare systems, adding to the challenges for governments amid tightened austerity budgets. It has now become more pressing than ever for countries to identify viable healthcare financing and delivery models that deliver on the promise of coverage for all.
“The sustainability of health financing is advanced by health system adaptations that either (1) achieve comparable health outcomes at a lower cost, or (2) achieve superior health outcomes at the same cost.”
— Professor David E. Bloom, Clarence James Gamble Professor of Economics and Demography from Harvard T.H.Chan
Drawing on our Southeast Asia sustainable health system financing efforts, here are a number of solutions that do more with less. The concepts then fall into two buckets: resolving the inefficiencies of existing resource allocation, and then applying a layer of creativity to the core system design.
Resolve the inefficiencies in the existing system
1. Healthcare is not just a cost item
One of the most common misalignments is how healthcare is often viewed as solely a cost item, leading to myopic investments. A paradigm shift is required for APAC countries to fully realize the potential of its policy measures.
Governments must see healthcare as a fundamental driver of socioeconomic ambitions and evolve from “health-for-all” to “health-to-wealth”.
For those countries seeking to capitalize on their demographic dividend period, and especially for those seeking to exit the middle-income trap, the time for more strategic investment decisions is now.
2. Prevention, prevention, prevention
A key opportunity is investment in cost-effective healthcare services such as preventative solutions.
Preventative solutions like life-course immunisation has proven to yield a return of $44 on every $1 spent on immunizations for families in low to middle income countries. According to the WHO, immunization saves 2-3 million deaths per year and is widely recognized as one of the world’s most successful and cost-effective health interventions. Unfortunately, many countries in the region fall short; they do not provide full coverage for adult-focused vaccines such as for seasonal influenza. APAC country leaders need to look past the “high” perceived cost and take a long-term approach in order to make savings in the long run.
3. Next-gen healthcare service delivery
Where traditional healthcare models struggle with gaps, there are alternatives.
For example, reinforcing primary care frees up hospitals (especially pertinent in the context of COVID), and promoting self-care and digital health tools reduces the strain on healthcare professionals (of which there is a shortage).
The pandemic has accentuated the role of digital health tools in overcoming the mobility and resource contraints faced by many countries. For example, China empowered the Internet Hospital in the fight against COVID-19.
Infectious diseases aside, self-care and digital health tools are also beneficial for patient pathways that require long-term self-maintenance such as Diabetes – a chronic disease with prevalence of as high as 40% in some Pacific island populations.
4. Cost policies that don’t compromise quality of care
Countries in the region can learn from Thailand, which rigorously adopted evidence-based purchasing policies such as Health Technology Assessment (HTA) to maximize the utilization of funds.
Many developed countries such as Canada and Taiwan have also increasingly adopted strategic purchasing for the reimbursement of healthcare services as well as products. They have moved away from payment mechanisms that use singular KPIs to determine reimbursement.
For instance in Canada, primary care medical attention is billed on a “fee-for-service” basis with additional “pay-for-performance” criteria such as the development of care plans and taking more time for patients with chronic or complex conditions. The approach helps to promote cost containment while not compromising the quality of care.
Revisit the core financing model to drive greater creativity
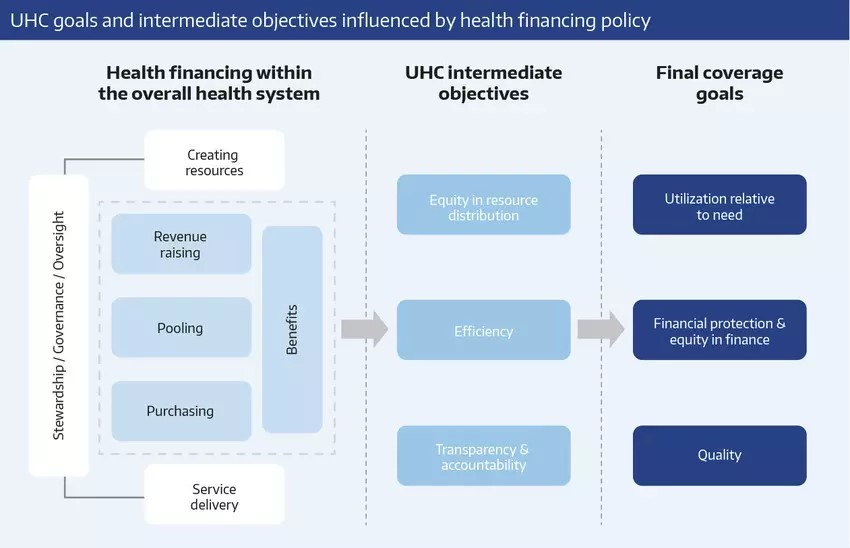
Given the growing demand that will continue to widen the gaps in health system financing and delivery, particularly during a pandemic, resolving the inefficiencies alone will not be sufficient. Governments must also revisit the core financing models being used in order to drive greater creativity in healthcare design.
1. Composite healthcare financing: taxes and social health insurance
To address the financing challenges faced by the region (shrinking taxable workforce and the presence of large informal economies), APAC should consider adopting a composite healthcare financing system that combines the best of both taxes and social health insurance, a model which has been implemented in Japan, for example.
Composite healthcare financing is certainly not a panacea, however. The structural weaknesses in APAC of tax collection and individual contributions must still be addressed, and various financing mechanisms need to be explored. One of the mechanisms could be to consider earmarking taxes or establishing nationalized funds for high impact disease and treatment areas like immunisation and RSV, the most common cause of hospitalization for Lower Respiratory Tract Infection (LRTI) in children younger than five years of age.
For example, Taiwan earmarked sin taxes to procure new vaccines for its national immunization programmes, while Bhutan invested its National Immunisation Fund so as to reap the returns from the interest rates.
2. Debt financing
Debt financing through public and private partnership in the form of Social Impact Bonds (SIBs), is another emerging novel financing mechanism in which private organizations invest in identified NGOs or public-sector programmes seeking to deliver a desired social outcome.
Once the social outcomes are achieved, the private organization will be repaid with the principle and returns. Such schemes have already been launched by Japan and Canada for diabetes and hypertension prevention.
3. Crowdfunding
Crowdfunding is yet another rising financing mechanism. In Singapore, the Rare Disease Fund (RDF) sees the government match public donations. Such mechanisms convert healthcare from “their problem” to “our collective passion”. The focus on rare disease truly honours the goal of Universal Health Coverage – leaving no one behind.
Above all, the journey to achieving sustainable healthcare in APAC can only be made possible with collective effort. Greater collaboration across public-sector agencies and among public-private partners is crucial to make the vision work. While there are challenges ahead, solutions do exist. But they need a greater collective effort from the healthcare funding ecosystem to see successful implementation in the APAC region.
Virtual ideation effort
With healthcare innovation upon us, there is always something to share and something to learn. Riding on the wave of crowdsourcing successes, Sanofi and KPMG are jointly launching a virtual ideation effort with the support of the World Economic Forum to gather innovative concepts that seek to revolutionize the healthcare delivery and financing models in APAC. These concepts will serve as inputs for our upcoming whitepaper due to launch in 2021.
The idea crowdsourcing will focus on four high impact thematic areas: Life Course Immunization, Diabetes Management, Respiratory Syncytial Virus (RSV), and Rare Diseases. Selected ideas will be credited in the whitepaper.
Read more about the sustainable healthcare programme here.
Source: www.weforum.org


